Middle East Respiratory Syndrome (MERS) is a viral respiratory illness caused by the MERS coronavirus (MERS-CoV). First identified in Saudi Arabia in 2012, MERS has since been a significant public health concern due to its high mortality rate and the potential for large-scale outbreaks, particularly in healthcare settings. This detailed article explores the pathology, clinical manifestations, transmission, prevention, and the critical role of the queue management system in hospital in controlling the spread of MERS.
Pathology and Clinical Manifestations
MERS is an infectious disease characterized by an acute and severe course. The virus induces an inflammatory process in the respiratory tract, which can lead to a range of symptoms from mild to severe, often with a serious prognosis.
Clinical Symptoms
- Asymptomatic to Mild Illness: Some individuals infected with MERS-CoV may be asymptomatic or exhibit mild respiratory symptoms.
- Moderate Illness: Typical symptoms include fever, cough, and shortness of breath. Pneumonia is common, but it does not always develop.
- Severe Illness: Severe cases can lead to acute respiratory distress syndrome (ARDS), requiring mechanical ventilation and intensive care unit (ICU) care. Gastrointestinal symptoms such as diarrhea can also be observed.
- High-Risk Groups: Older adults, people with weakened immune systems, and individuals with chronic conditions such as kidney disease, cancer, chronic lung disease, hypertension, cardiovascular disease, and diabetes are at increased risk of developing severe illness.
The most dangerous complications of MERS include ARDS, heart failure, and kidney failure, all of which significantly contribute to the high mortality rate associated with the disease.
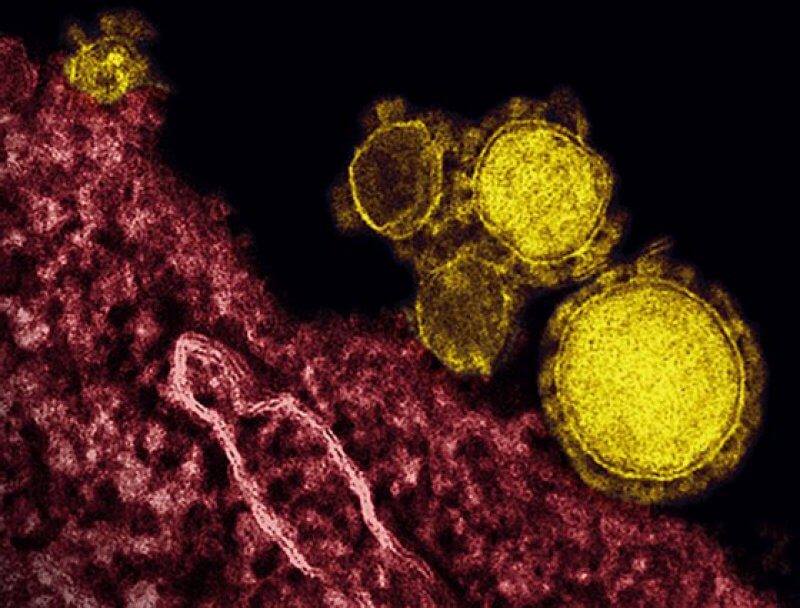
Pathogenesis and Virology
MERS-CoV is a zoonotic virus, meaning it is transmitted between animals and humans. It is part of the Coronaviridae family, which also includes the viruses responsible for Severe Acute Respiratory Syndrome (SARS) and Coronavirus Disease 2019 (COVID-19). The primary reservoirs for MERS-CoV are dromedary camels, which are believed to play a significant role in the transmission of the virus to humans.
Upon entering the human body, MERS-CoV targets epithelial cells in the respiratory tract. The virus attaches to the host cell’s surface receptor, Dipeptidyl Peptidase 4 (DPP4), and begins to replicate. This replication triggers an immune response, resulting in the inflammatory processes that characterize MERS. In severe cases, the immune response can become dysregulated, leading to a cytokine storm, which can cause ARDS and multi-organ failure.
Mortality Rate
Approximately 35% of reported MERS cases result in death. However, this figure may overestimate the actual mortality rate, as mild cases often go undetected by current surveillance systems. The high mortality rate is particularly concerning given the potential for severe complications and the strain they place on healthcare resources.

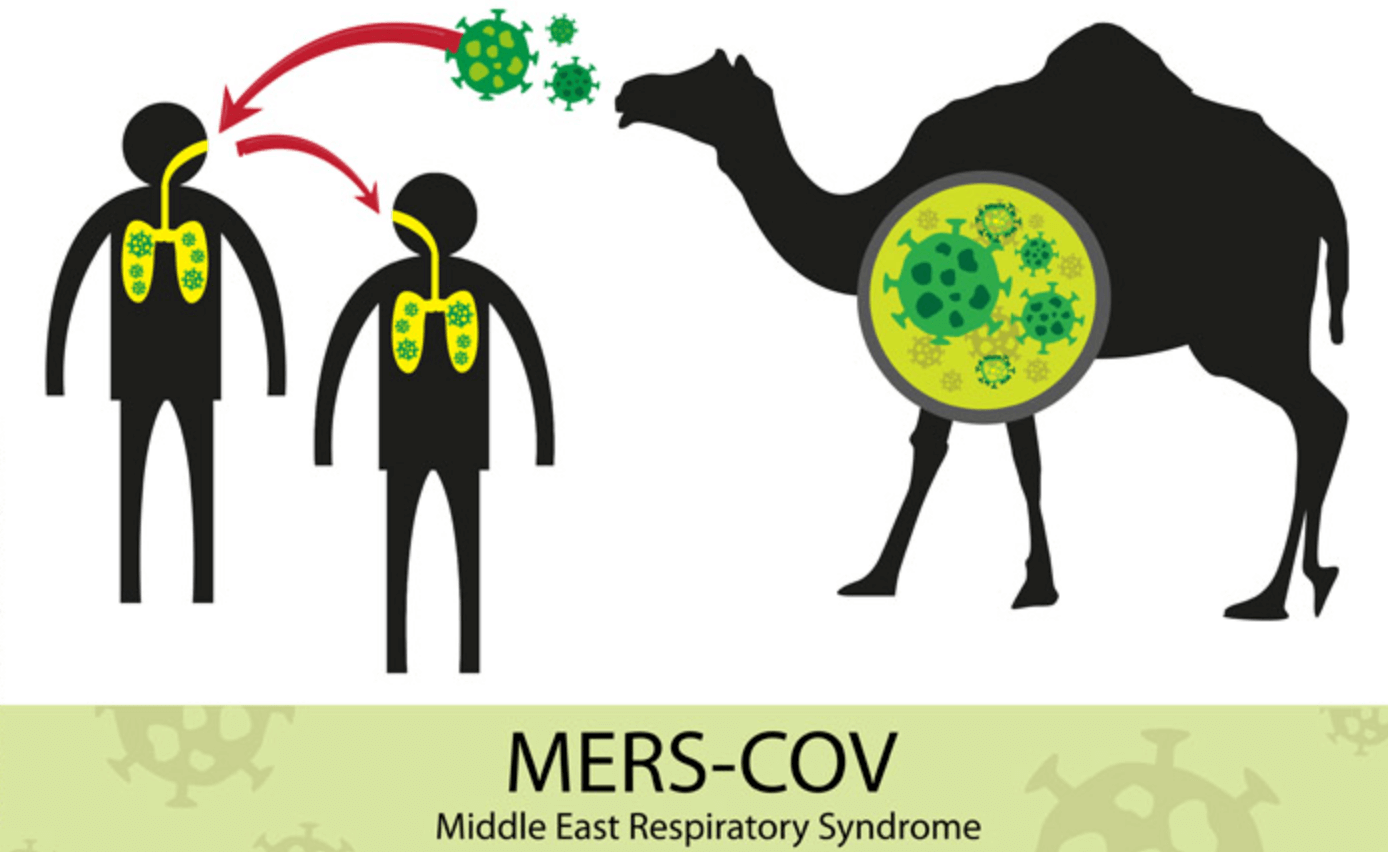
Transmission of MERS-CoV
MERS-CoV primarily spreads through close contact and exposure to respiratory secretions. Transmission is most common in healthcare settings, where patients, healthcare workers, and visitors are at high risk.
- Healthcare Settings: The largest outbreaks have occurred in hospitals in Saudi Arabia, the United Arab Emirates, and South Korea.
- Household Transmission: Family members and others living in close quarters with an infected person are also at risk.
No country has documented sustained person-to-person transmission outside healthcare settings.
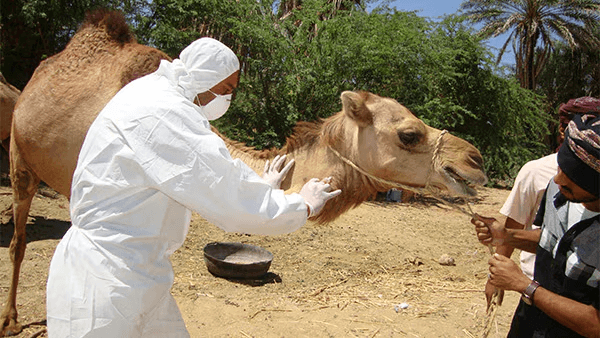
Animal-to-Human Transmission
In addition to human-to-human transmission, MERS-CoV can be transmitted from animals to humans. Camels are considered the primary source of infection for humans. People in close contact with camels, such as herders and those consuming camel products, are at higher risk of contracting MERS-CoV.
Preventive Measures
Preventing the spread of MERS involves both specific and non-specific measures:
- Travel Precautions: Travelers to countries with known MERS cases should use protective masks and avoid crowded places.
- General Hygiene: Regular hand washing, avoiding contact with sick animals, and ensuring proper food safety (e.g., avoiding raw camel milk and undercooked meat) are crucial.
- Home and Personal Hygiene: Regular ventilation, wet cleaning, and personal hygiene practices can reduce the risk of transmission.
- Healthcare Measures: In case of symptoms of acute respiratory viral infections (ARVI), wearing masks and seeking immediate medical help is advised. Reporting travel history to healthcare providers is essential for early detection and management.
- Public Health Measures: Governments and health organizations recommend routine surveillance and rapid diagnostic testing to quickly identify and isolate cases. Educating the public about MERS and encouraging prompt reporting of symptoms are also critical steps in preventing the spread.
The Role of Hospital Queue Management Systems
An effective queue management system in hospitals is vital in preventing the spread of MERS and protecting both patients and healthcare workers. Here are key aspects of its importance:
Minimizing Close Contact
Queue management systems can minimize the amount of time patients spend in crowded waiting areas, reducing close contact and the risk of person-to-person transmission.
Efficient Patient Flow
By streamlining patient flow and ensuring timely access to medical services, these systems can prevent bottlenecks that increase the risk of transmission in healthcare settings.
Isolation and Prioritization
Queue systems can help prioritize patients based on the severity of their symptoms and their potential infectiousness. Patients suspected of having MERS can be quickly isolated and given appropriate care, thereby reducing the risk of spreading the virus to other patients and healthcare workers.
Tracking and Monitoring
Hospital queue management systems can keep track of patient movements and interactions within the facility, aiding in contact tracing efforts if an outbreak occurs. This data is crucial for identifying and isolating potential cases swiftly.
Reducing Anxiety and Improving Compliance
A well-organized queue management system can reduce patient anxiety by providing clear information about wait times and procedures. This can lead to better compliance with infection control measures, such as wearing masks and maintaining physical distance.
Challenges and Future Directions
Despite advances in understanding and managing MERS, several challenges remain:
- Limited Treatment Options: Currently, there is no specific antiviral treatment for MERS-CoV. Supportive care remains the primary treatment modality, focusing on relieving symptoms and managing complications.
- Vaccine Development: Developing an effective vaccine against MERS-CoV is a priority, but progress has been slow. Several vaccine candidates are in various stages of development and testing.
- Global Surveillance and Response: Enhancing global surveillance systems and ensuring rapid response capabilities are crucial for early detection and containment of MERS outbreaks.
Conclusion
Middle East Respiratory Syndrome remains a significant public health challenge due to its high mortality rate and potential for severe complications. Understanding the pathology, clinical manifestations, and transmission routes is crucial for managing and preventing outbreaks. Implementing effective preventive measures and utilizing advanced hospital queue management systems are essential steps in controlling the spread of MERS and protecting public health. Through continued vigilance, research, and international cooperation, we can better address the threats posed by MERS and improve our readiness for future infectious disease outbreaks.
MERS exemplifies the ongoing battle between emerging infectious diseases and public health efforts to contain them. As we continue to learn more about this disease, it is imperative to maintain robust healthcare systems, advance scientific research, and foster global collaboration to mitigate the impact of such infectious threats.

Hockey fan, nature enthusiast, music blogger, vintage furniture lover and multidisciplinary designer. Doing at the intersection of art and mathematics to craft experiences that go beyond design.